In the 1980s, researchers discovered that patients with celiac disease had high levels of antibodies that recognized gliadin (a protein in gluten) in their small intestine.1 Patients with celiac disease were also found to have auto-reactive antibodies—that is, antibodies that recognize normal “self” proteins.
Researchers developed a blood test that was able to detect IgA antibodies that recognized a type of tissue called endomysium.2 In 1997, Dr. Detlef Schuppan and his team discovered that IgA antibodies in the blood of patients with celiac disease recognized a specific protein in the endomysium—a protein called tissue transglutaminase (tTG).3 The antibodies to gliadin, endomysium, and tTG disappear when patients adopt a gluten-free diet, which suggests that these antibodies are made as part of an immune response to gluten.
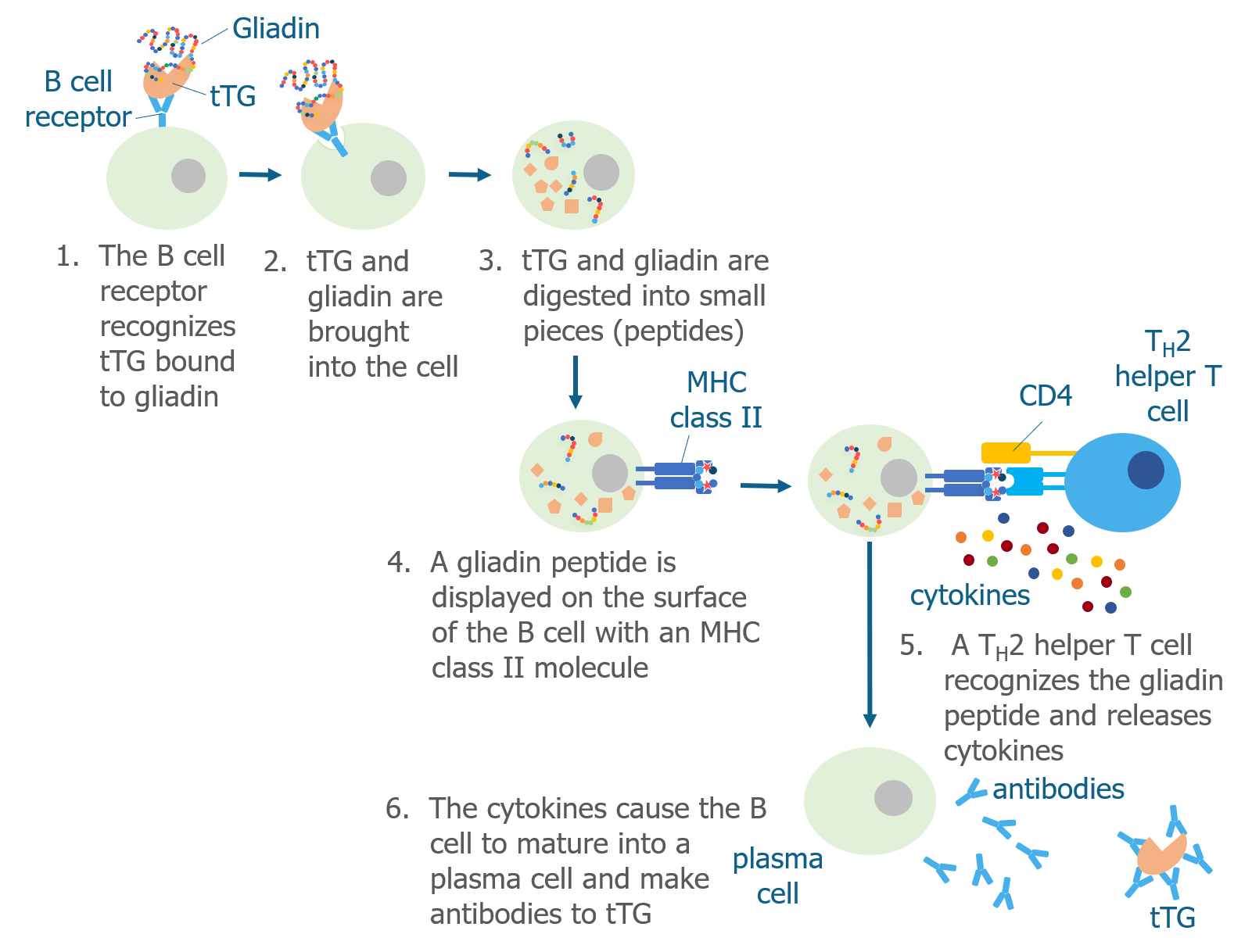
We know that T cells can recognize deamidated gliadin peptides and begin an immune response, so it makes sense that B cells might produce antibodies to gliadin if they mistakenly recognize it as a pathogen. But why would B cells produce antibodies to tTG, a normal protein in the body?
As we discussed above, tTG is the enzyme that is responsible for converting the glutamine amino acids into glutamate amino acids to produce deamidated gliadin peptides, which have increased immunogenicity. In addition to changing glutamines to glutamates, tTG can also cross-link the gluten peptide to itself.
Researchers are still trying to understand exactly how gluten causes B cells to make antibodies that recognize tTG, but they think that B cells ingest tTG that is cross-linked to a gliadin peptide. Then, Th2 helper T cells that recognize gliadin help B cells produce antibodies to tTG.
REFERENCES
- Mesin L, Sollid LM, Di Niro R. The intestinal B-cell response in celiac disease. Front Immunol. 2012;3:313.
- Chorzelski TP, Sulej J, Tchorzewska H, Jablonska S, Beutner EH, Kumar V. IgA class endomysium antibodies in dermatitis herpetiformis and coeliac disease. Ann N Y Acad Sci. 1983;420:325-334.
- Dieterich W, Ehnis T, Bauer M, et al. Identification of tissue transglutaminase as the autoantigen of celiac disease. Nat Med. 1997;3(7):797-801.
GLOSSARY
Antibodies – Y-shaped proteins that recognize foreign pathogens. Made by B cells. Also called immunoglobulins.
B cell – A type of adaptive immune cell. Also called B lymphocyte.
Endomysium – A type of connective tissue.
Enzyme – A protein that can change one type of molecule to another.
Gliadin – One of the wheat proteins that forms gluten. Responsible for triggering an immune response in patients with celiac disease.
Gluten – A type of protein found in cereal grains. Wheat gluten is made of two proteins called gliadin and glutenin.
Helper T cell – Adaptive CD4+ immune cell that produces cytokines when activated.
Immunogenicity – The ability of an antigen to induce an immune response.
T cell – A type of adaptive immune cell. Also called T lymphocyte.
Tissue transglutaminase (tTG) – An enzyme that deamidates gliadin peptides causing them to be more immunogenic. Also the target of auto-antibodies in patients with celiac disease.
RELATED
Celiac Disease: Biology Basics
May 17, 2018What Happens In the Small Intestine?
May 6, 2018B Cells
May 6, 2018What Role Does Tissue Transglutaminase (tTG) Play in Celiac Disease?
May 6, 2018Share this Post