In the 1960s and 1970s, researchers began to understand that the immune system was involved in celiac disease, and that the immune response occurred upon exposure to gluten.1
One of the first clues was that more lymphocytes were found in the intestines of patients with untreated celiac disease and fewer lymphocytes were found in the intestines of patients who were following a strict gluten-free diet. Another clue to the importance of the immune system in celiac disease was the discovery that patients with celiac disease had antibodies to wheat proteins circulating in their bloodstream.2
By the 1980s and 1990s, researchers understood that T cells (adaptive immune cells) were involved in the immune response to gluten and the development of celiac disease.3-5 They also understood that B cells made antibodies that recognized a normal protein in the intestine called tissue transglutaminase or tTG.6
In the next sections we will learn more about the roles that T cells and B cells play in celiac disease.
T Cells
Like all immune cells, T cells have receptors (in this case called T cell receptors) that recognize antigens. Once the antigen is recognized, the T cell becomes activated. Activated T cells are responsible for destroying the pathogen, either directly by killing the infected cell, or indirectly by activating B cells or innate immune cells—this is often called the cell-mediated immune response.
How do T cells recognize antigens?
Unlike other immune cells, T cells are not able to recognize antigens on their own. The antigens have to be presented to them in a way that allows the T cell receptor to recognize them.
Antigens can be presented to T cells in one of two ways: 1) by normal cells that are infected; or 2) by professional antigen presenting cells.
Infected cells
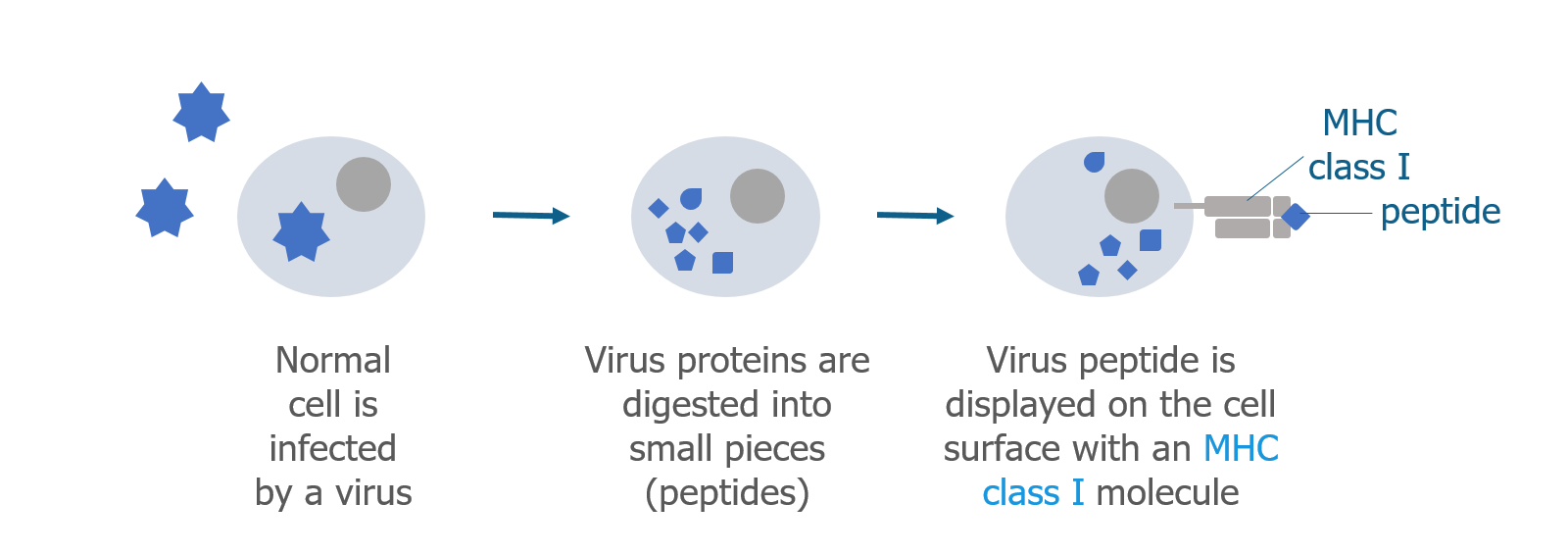
Cells normally break down proteins and make new ones to replace them. Many cellular proteins are broken down into smaller pieces called peptides. Some of these peptides are sent to the surface of the cell along with a major histocompatibility complex (MHC) class I protein. The MHC class I protein displays the peptide on the outside of the cell so it can be recognized by certain T cells. If a cell has been infected by a foreign pathogen, such as a virus that lives inside the cell, viral peptides (antigens) will be displayed on the surface of the infected cell.
Antigen presenting cells
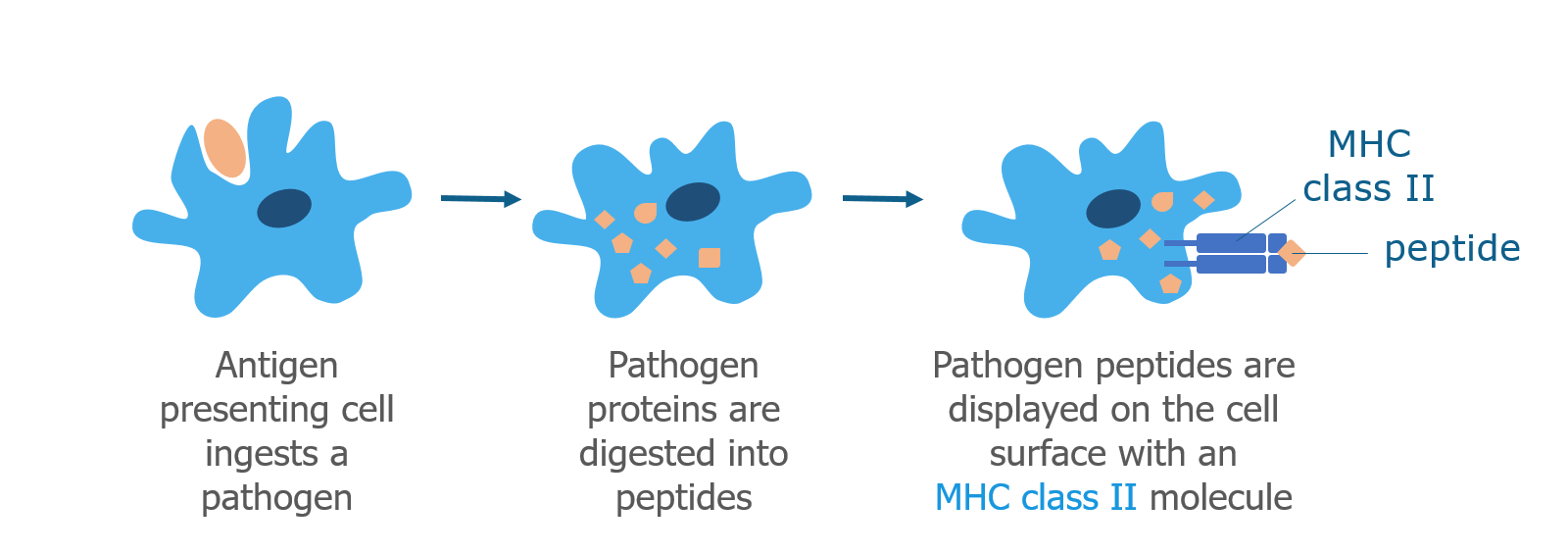
Dendritic cells, macrophages, and B cells are professional antigen presenting cells that process pathogens. When an antigen presenting cell bumps into a pathogen, it brings it inside the cell using a process called phagocytosis (cell eating). Similar to normal cellular proteins, the pathogen is digested into peptides, which are displayed on the surface of the cell together with a MHC class II protein. Like the MHC class I protein, the MHC class II protein displays the peptide (antigen) and interacts with certain T cells.
What Are the Different Types of T Cells?
Cytotoxic T cells (CD8+)
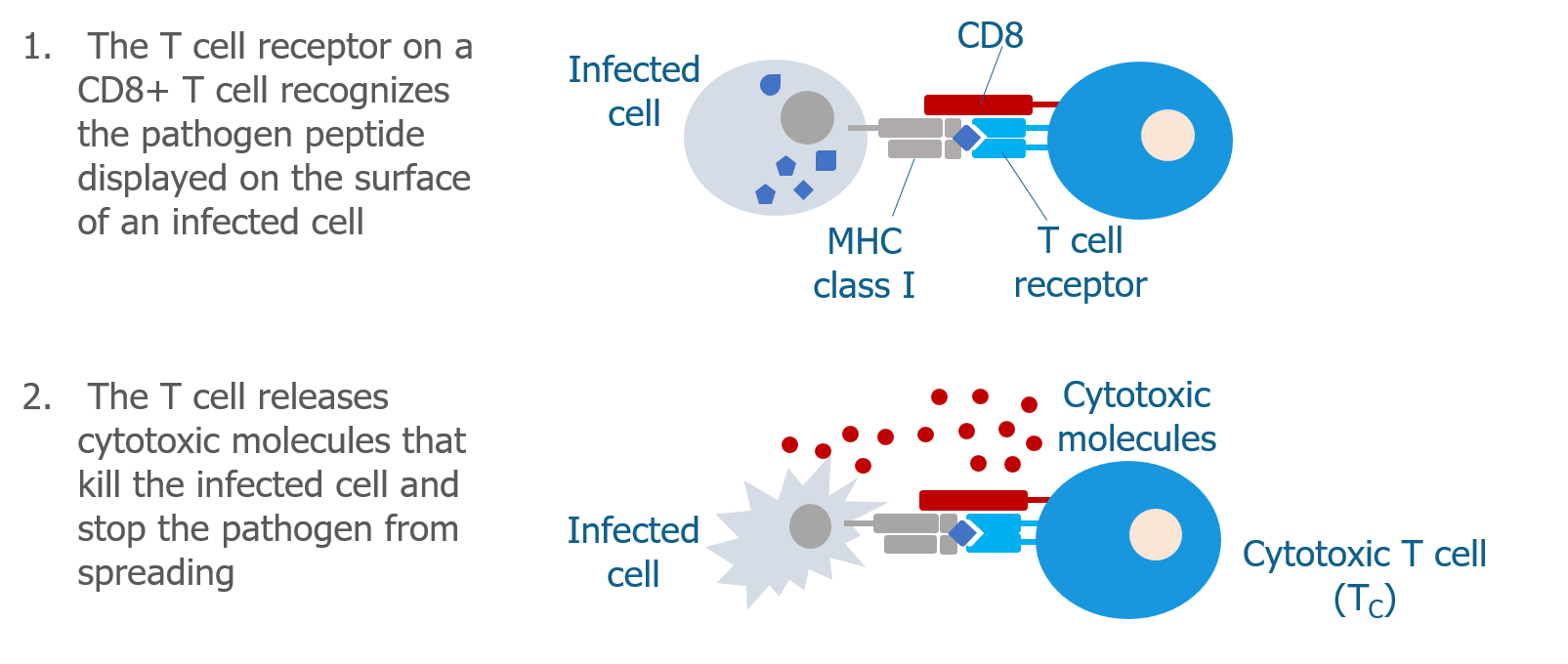
Cytotoxic T cells (Tc cells) have a co-receptor called CD8 on their cell surface. CD8 partners with the T cell receptor and with MHC class I molecules, acting as a sort of bridge. This bridge allows cytotoxic T cells to recognize normal cells that are infected by a pathogen. When the cytotoxic T cell recognizes the infected cell, it becomes activated and produces molecules that kill the infected cell, destroying the pathogen in the process.
Helper T cells (CD4+)
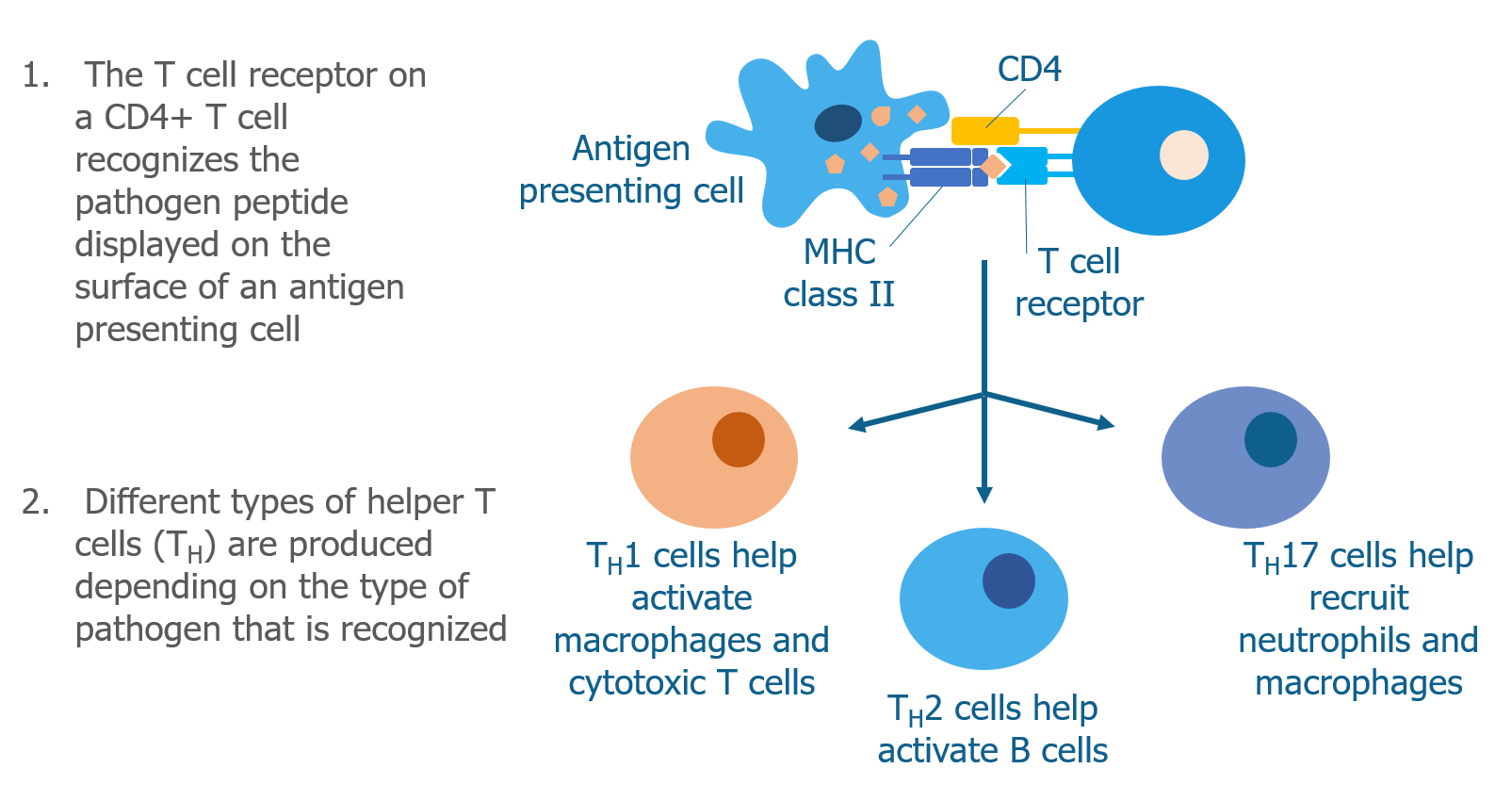
Helper T cells (Th cells) have a different co-receptor called CD4 on their cell surface. CD4 also partners with the T cell receptor but interacts with MHC class II molecules instead of MHC class I molecules. This allows helper T cells to recognize pathogen peptides that have been displayed by antigen presenting cells. When helper T cells recognize a peptide on an antigen presenting cell, they become activated and begin to produce molecules called cytokines that signal to other immune cells.
There are many subtypes of helper T cells (ie, Th1, Th2, Th17). Each subtype produces a specialized combination of cytokines that depends on type of pathogen that the helper T cell has recognized—some cytokines are more effective than others in the process of eliminating certain invaders.
Regulatory T cells
Regulatory T cells (Treg cells) also have CD4 on their surface, but they do not activate the immune system like helper T cells do. Instead, regulatory T cells play a protective role by shutting off the immune response when it is no longer needed. This prevents excessive damage to the normal cells and tissues in the body. Regulatory T cells suppress the immune response in several ways, including:
- Producing anti-inflammatory cytokines that suppress the immune response
- Releasing molecules that kill activated immune cells
- Changing the way dendritic cells behave so they can’t activate T cells
Which T cells are involved in celiac disease?
Of the 3 types of T cells described above, the CD4+ T helper cells play a leading role in celiac disease. These are the cells that mistakenly recognize gluten as a pathogen and trigger an immune response (see below).7 However, cytotoxic CD8+ T cells known as intraepithelial lymphocytes (IELs) are also important as they are drivers of tissue damage in the intestine.8
How Does Gluten Activate T Cells?
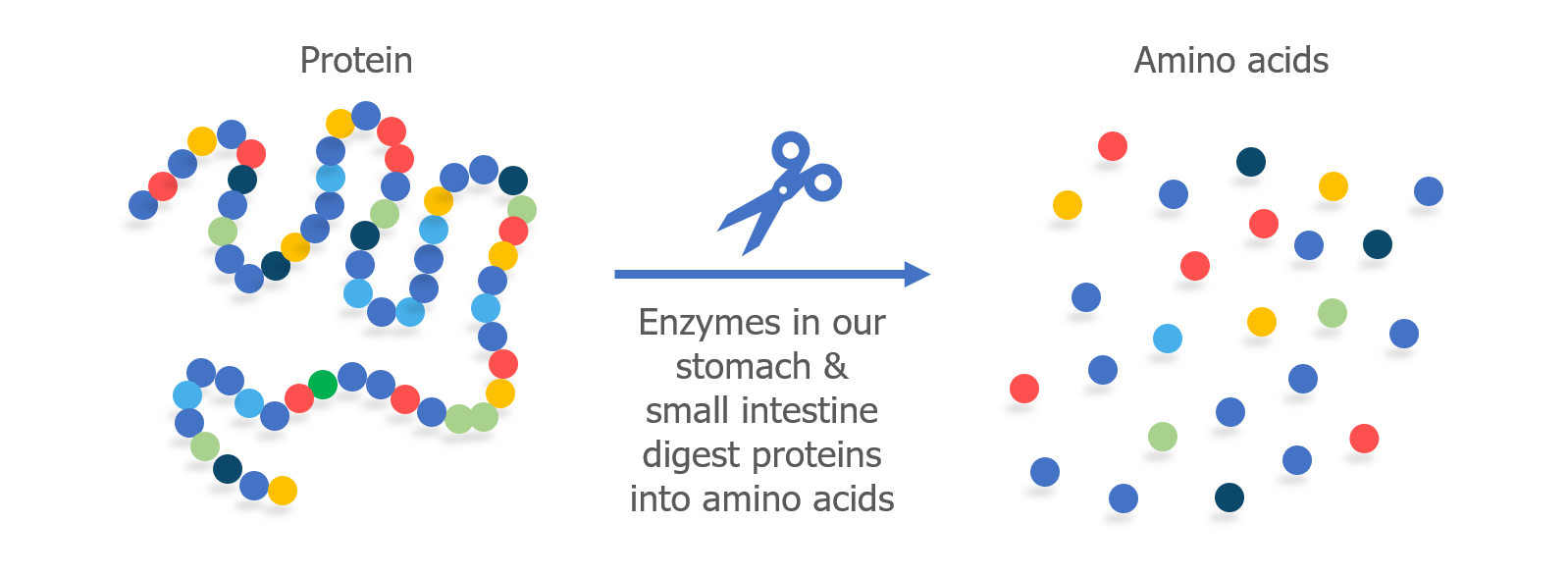
All proteins are made up of smaller parts called amino acids. The amino acids are linked together to form a long chain, like beads that have been strung together to form a necklace.
When we eat protein, enzymes in our digestive system (called proteases) break apart the chain into individual amino acids. In our intestine, cells called enterocytes absorb the amino acids so they can be used to fuel our bodies and rebuild our own proteins.
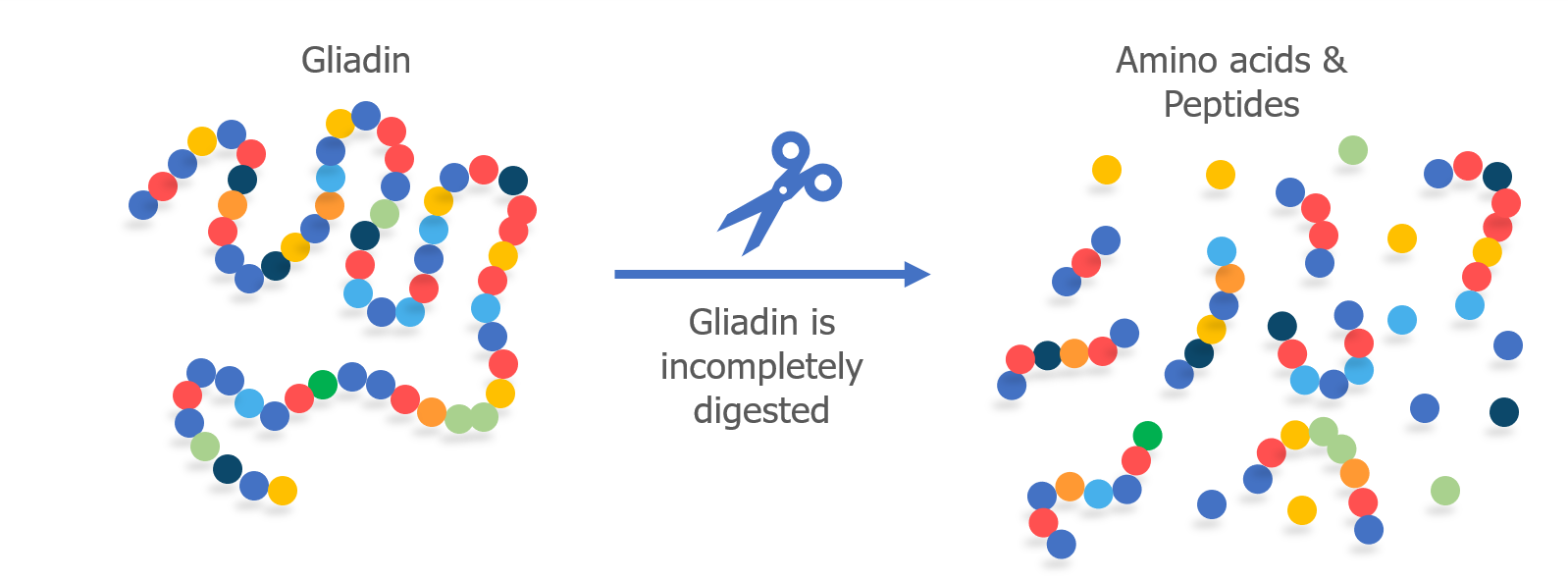
When humans eat gluten, it is not completely digested into individual amino acids in the small intestine. Gliadin, specifically, is difficult for our bodies to digest because it contains a high proportion of two amino acids—proline and glutamine. Because it is only partially digested, small fragments of the gliadin protein chain remain as peptides. This happens in people with and without celiac disease.
Antigen presenting cells located in the intestine take up the undigested gliadin peptides and display them on their surface with an MHC class II molecule. CD4+ T cells with receptors shaped like “locks” that match gliadin peptide “keys” mistakenly recognize gluten as a harmful pathogen and become activated. This begins the immune response.
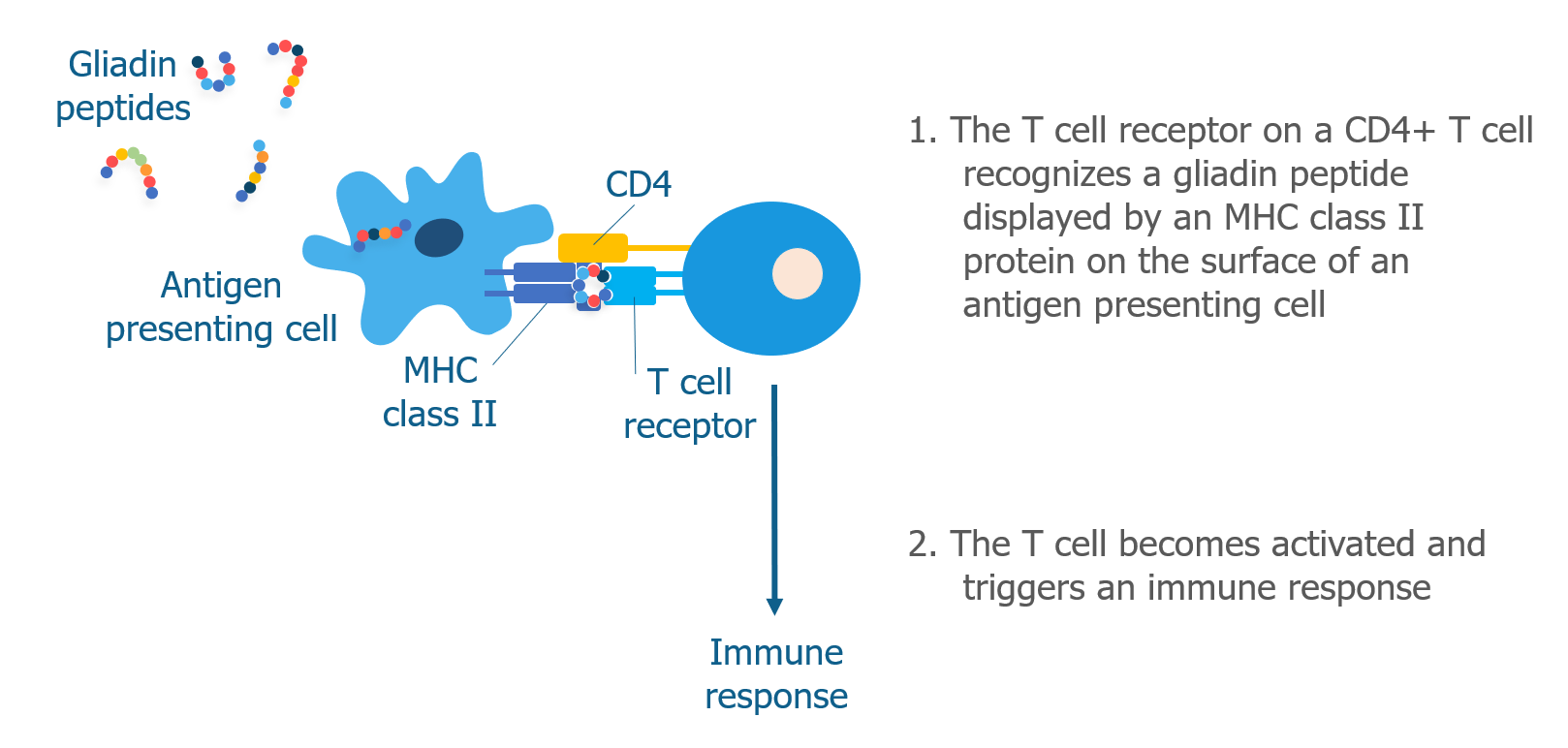
Once CD4+ T cells become activated, they can produce different subsets of helper T cells (as described here). In celiac disease, the most common type of helper T cell produced is Th1, which produces cytokines, such as interferon gamma, that recruit other immune cells and cause tissue damage. There is also evidence for Th17 cells in celiac disease. Th17 cells produce interleukin-17, which is a key cytokine involved in several different autoimmune diseases.7
NEXT TOPIC: What does it mean to be genetically predisposed?
REFERENCES
- Ferguson A, Murray D. Quantitation of intraepithelial lymphocytes in human jejunum. Gut. 1971;12(12):988-994.
- Kowlessar OD. Effect of wheat proteins in celiac disease. Gastroenterology. 1967;52(5):893-897.
- Halstensen TS, Scott H, Farstad IN, Michaelsen TE, Brandtzaeg P. In situ two- and three-color immunofluorescence staining of mucosal T-cells in celiac disease. Increase of TCR gamma/delta+CD8- and TCR alpha/beta+CD45R0+ intraepithelial lymphocytes and IL-2R+ TCR alpha/beta+CD4+CD45R0+ lamina propria lymphocytes. Prog Histochem Cytochem. 1992;26(1-4):201-210.
- Marsh MN. Gluten, major histocompatibility complex, and the small intestine. A molecular and immunobiologic approach to the spectrum of gluten sensitivity (‘celiac sprue’). Gastroenterology. 1992;102(1):330-354.
- Selby WS, Janossy G, Bofill M, Jewell DP. Lymphocyte subpopulations in the human small intestine. The findings in normal mucosa and in the mucosa of patients with adult coeliac disease. Clin Exp Immunol. 1983;52(1):219-228.
- Dieterich W, Ehnis T, Bauer M, et al. Identification of tissue transglutaminase as the autoantigen of celiac disease. Nat Med. 1997;3(7):797-801.
- Jabri B, Sollid LM. T Cells in Celiac Disease. J Immunol. 2017;198(8):3005-3014.
- Abadie V, Discepolo V, Jabri B. Intraepithelial lymphocytes in celiac disease immunopathology. Semin Immunopathol. 2012;34(4):551-566.
GLOSSARY
Adaptive immune cells – Immune cells that recognize specific pathogens. Allow the immune system to “remember” pathogens in case of future infection.
Amino acids – Small units that are linked together by bonds to form proteins.
Antibodies – Y-shaped proteins that recognize foreign pathogens. Made by B cells. Also called immunoglobulins.
Antigen – A protein that is recognized by an immune cell receptor and triggers an immune response.
Antigen presenting cell – A specialized immune cell that presents peptides to CD4+ or CD8+ T cells. Peptides are presented by MHC I or MHC II proteins.
B cell – A type of adaptive immune cell. Also called B lymphocyte.
CD4 – A co-receptor on the surface of helper T cells.
CD8 – A co-receptor on the surface of cytotoxic T cells.
Cell-mediated immune response – Immune response that involves the direct or indirect activation of immune cells.
Cytokines – Small proteins that are made and released by immune cells. Allows cells to send signals and provide instructions to other cells.
Cytotoxic T cell – Adaptive CD8+ immune cell that kill infected cells when activated.
Enterocytes – Cells that make up the intestinal lining. Responsible for absorbing nutrients.
Gliadin – One of the wheat proteins that forms gluten. Responsible for triggering an immune response in patients with celiac disease.
Gluten – A type of protein found in cereal grains. Wheat gluten is made of two proteins called gliadin and glutenin.
Helper T cell – Adaptive CD4+ immune cell that produces cytokines when activated.
Immune cells – Specialized white blood cells (also called leukocytes) that fight infection.
Innate immune cells – Nonspecific immune cells. Recognize many pathogens. First responders to infection.
Intraepithelial lymphocytes – Cytotoxic CD8+ T cells that reside in the intestine. Contribute to tissue damage in celiac disease.
Lymphocyte – Adaptive immune cells. Can by B or T lymphocytes.
MHC class I protein – Major histocompatibility complex class I protein. Found on the surface of normal cells. Presents peptides to CD8+ T cells.
MHC class II protein – Major histocompatibility complex class II protein. Found on the surface of antigen presenting cells. Presents peptides to CD4+ T cells.
Pathogens – Bacteria and viruses that can cause disease.
Peptide – A small protein fragment consisting of a chain of amino acids.
Protease – A type of enzyme that breaks up proteins into smaller parts.
Receptor – A protein that is located on the surface of a cell and interacts with other proteins. Receptors act as the “locks” that recognize specific pathogen “keys”.
Regulatory T cell – An adaptive immune cell that suppresses the immune response.
T cell – A type of adaptive immune cell. Also called T lymphocyte.
Tissue transglutaminase (tTG) – An enzyme that deamidates gliadin peptides causing them to be more immunogenic. Also the target of auto-antibodies in patients with celiac disease.
Share this Post